You are here

Who’s first wins? International crisis response to Covid-19
Introduction
The Covid-19 pandemic appears to be not just a test for healthcare systems around the world, but an international contest for which country has the best political system. As the People’s Daily, the official mouthpiece of the Chinese Communist Party (CCP), boasted in an article published in early March, “China’s battle against the epidemic showed that the CCP, as China’s ruling party, is by far the political party with the strongest governance capability in human history.”1 It pointed the finger at Europe for “acting too little and too late, and largely failing to stem the tide”.2 Slow response time, high rates of transmission, and a general unwillingness to impose restrictive emergency measures were ascribed to the inherent deficiencies of open democratic, liberal systems, making them appear unfit to deal with health crises or indeed for governance generally.
In this Brief, we put this hypothesis to the test: did democracies really respond less swiftly than authoritarian systems – and if the determining factor is not the political system, what are the key elements in crisis response?
Data: WHO,2020; The New York Times, 2020
Critical time lags
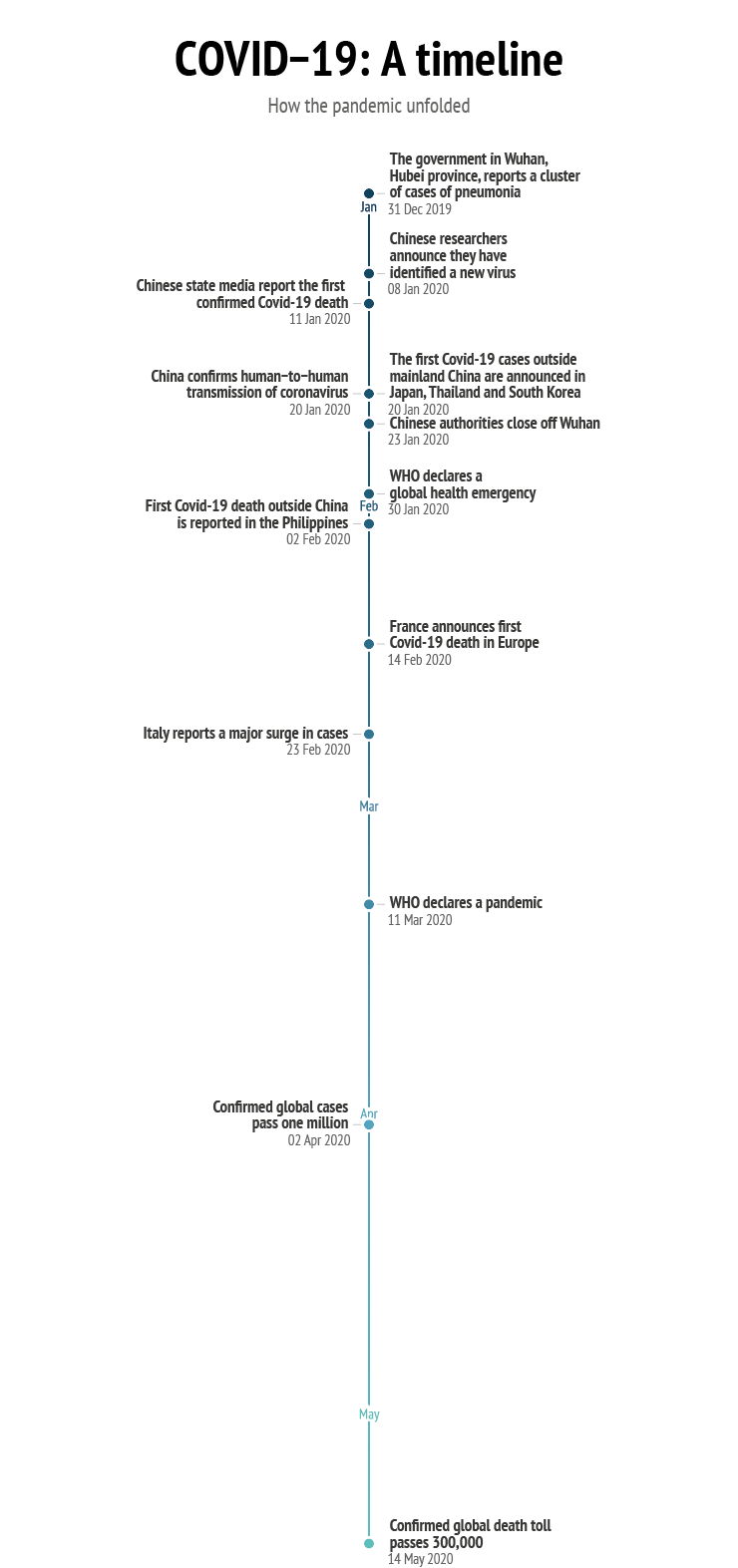
Response time is one of the main yardsticks for gauging the efficiency of a crisis management system. But at what stage is a crisis perceived as such? It is much easier to point to the beginning of a crisis in hindsight. In the case of Covid-19, this is complicated further by the fact that non-democratic regimes have less transparent reporting mechanisms: China, for instance, has a history of editing the statistics it releases to the outside world, starting with GDP figures.3 Although it reported its first case of the disease to the World Health Organisation (WHO) on 31 December (but claimed it could not confirm human-to-human transmission), there is reasonable doubt over whether this was actually indeed the first case, as reports subsequently emerged that Beijing had silenced whistle-blowers. Moreover, the latest evidence suggests that the virus had spread to Europe before that date.4 This lack of transparency in turn affected others further down in the information chain: on 17 January, the European Centre for Disease Prevention and Control (ECDC), which had monitored the situation for two weeks already, noted that “in the absence of detailed information from the ongoing studies in China, it is impossible to quantify the potential of the 2019-nCoV for human-to-human transmission.”5 Only on 20 January did China confirm human-to-human transmission, whereupon the ECDC elevated the potential impact of the 2019-nCoV outbreak to ‘high’ and considered a global spread of the disease to be ‘likely’.
Data: various news sources
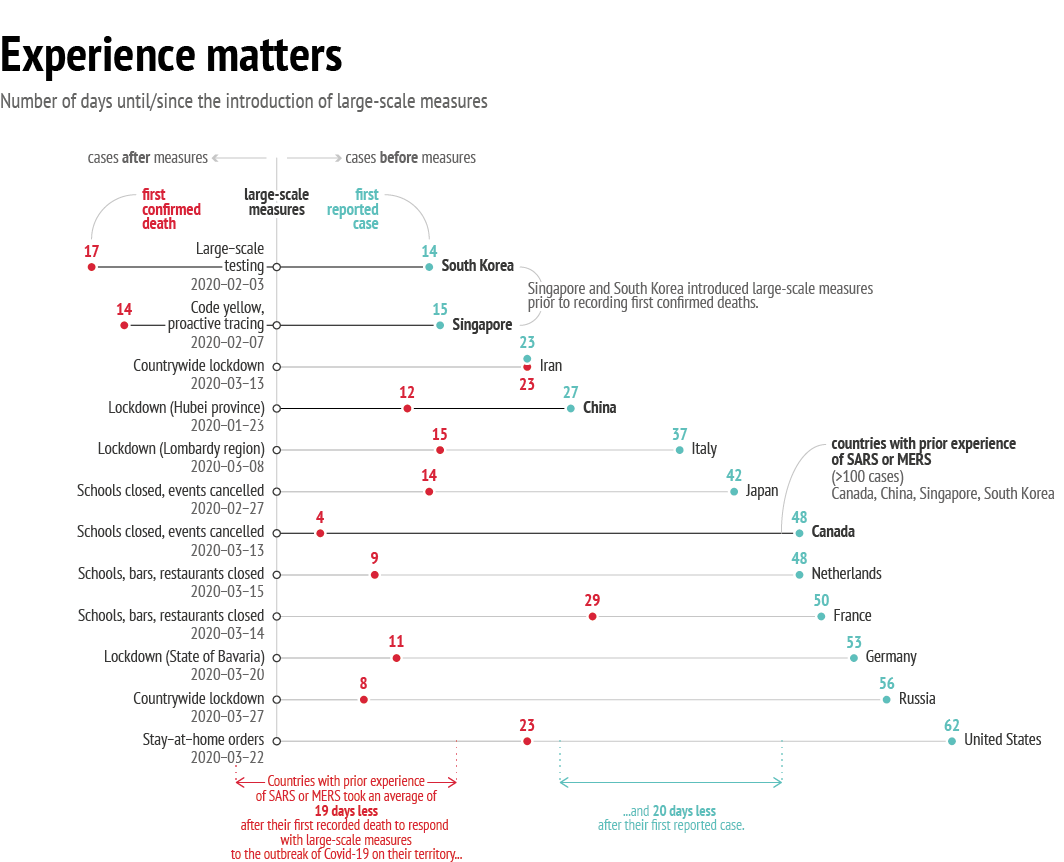
Nevertheless, if response time is measured as the number of days between the first confirmed case and the introduction of emergency measures, the picture shows South Korea and Singapore ahead of China.This means that the time lag between the first case and measures taken in response varied greatly between political systems.
Another criterion for measuring response time is the pace with which the virus spread, i.e. the number of days it took for the number of cases to grow exponentially. The slower the rate, the more governments were seen as successful in ‘flattening the curve’, i.e. in delaying infection rates.
The number of infections, too, is difficult to measure because of the wide variations from country to country in the amount of testing carried out, while the assumption that only one strain of the virus exists is also problematic. Evidence seems to suggest that Covid-19 has two, or even more, variants: one, located deep in the lungs, is more lethal but less contagious, whereas another is located in the throat – less lethal, but more contagious. The rate of transmission depends therefore also on which strain of the virus is circulating in a given country or region.6 One thing that is noticeable, however, is that there was a particularly high rate of infection in countries that were affected earlier on in the crisis: in China and Italy the number of days between the first and hundredth recorded Covid-19 case stands at 23, and in Iran at only 7. In other Asian countries and Western Europe, there was a time interval of between 30 and 40 days between the first detected case and the hundredth recorded case; and in North America and Russia the interval between case 1 and 100 was even longer. This means that states that were affected later on had more time to take precautionary measures and thus a better chance of slowing down the pandemic – no matter what their political system. Even so, exponential growth – i.e. the speed with which the virus spreads – is not easily understood by the human mind. Most mathematical problems we encounter are not of an exponential nature, meaning that exponential growth of such magnitude makes it difficult for us to grasp the true scale of the problem at hand.
Another way to measure response time would be to count the days between the first reported death from Covid-19 and the introduction of emergency restrictive measures. When measured this way, South Korea and Singapore again lead the field as they took measures more than two weeks before they recorded the first death. Right behind them is Canada, another democratic state. China’s response time following the first death is behind that of Germany, the Netherlands, and Russia – and almost on a par with Italy. In fact, China failed rather conspicuously in terms of promptness of response: it allowed more than 7 million people to leave Wuhan – the epicentre of the virus – between the start of the outbreak and the introduction of the travel ban three weeks later. As a result, the virus had spread to major cities such as Shanghai and Beijing – and, most importantly, it had begun to reach other countries, with the first case being reported in Thailand in mid-January. A few days later – two days after China imposed its travel ban – cases appeared in Singapore, Hong Kong and the United States. What we now know is that the virus had already spread by then to 30 cities across 26 countries from Wuhan alone.7
No matter how the efficacy of its response is measured, China clearly did not act faster than the democratic systems it has accused of being slow in reacting to the pandemic.
Not my problem? The evolution of crisis awareness
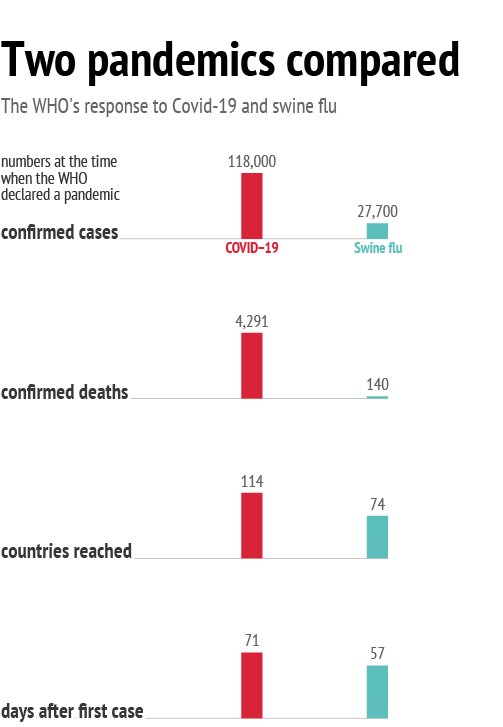
But are the first deaths alone sufficient to trigger awareness of the seriousness of a pandemic? After all, the swine flu, too, that spread globally in 2009 infected as many as 1.4 billion people while displaying low lethality rates of about 0.02%.8 As late as the beginning of March, Covid-19’s lethality was not widely understood, with estimates ranging between 1 and 2%.9 Only in mid-March, when fatality rates in Italy exceeded 6%, did public awareness of the severity of the virus begin to grow. Since then, the virus’s fatality rate has fluctuated depending on country and testing methods, ranging from 20% in France, to between 12% and 16.4% in Spain, the Netherlands, Sweden, Belgium and Italy, around 7.5% in China, Iran, Ireland, Canada and the US. Meanwhile, fatality rates stand at just under 5% in Germany, Finland, and Japan, and between 0.08% and 2.4% in Singapore, South Korea and Russia.10 As the fatality rate reflects the ratio between confirmed deaths and confirmed cases, the number of tests performed per country to confirm cases matters greatly. But there are also wide variations between countries in terms of the amount of testing carried out.11
Once the speed with which the virus was spreading, and its fatality rate, became clear, it still took several governments a number of days to implement emergency measures despite intense media reporting. This may have been due to psychological factors at play: because pandemics generally receive a lot of media attention (particularly when accompanied by alarming symptoms), there is a danger of ‘warning fatigue’ setting in among the public – and indeed the authorities. Constant exposure to a threat, somewhat ironically, may mean that it is no longer perceived as such.12 In the case of Covid-19, with symptoms resembling Severe Acute Respiratory Syndrome (SARS) and swine flu (neither of which seriously affected Europe), it was not novel, and the symptoms did not appear to be particularly severe. The likelihood of the virus reaching Europe was probably perceived accurately, but the lethality and speed of the virus were underestimated both by the media and by decision-makers. Covid-19 also shows us that threat perception does not increase at the same speed as the threat itself: when a disease affects a state far away, people will automatically tend to assume that it does not pose a direct threat.
Learning from the past
So how come other states acted before the full extent of the pandemic was known? The answer lies in their past first-hand experience of a similar health crisis – not the swine flu (which was very contagious but not very lethal), but SARS, a not very contagious but highly lethal coronavirus with a fatality rate of 14%.13
Data: WHO, 2020; The Guardian, 2009
When measured this way, it becomes clear that the main element triggering swift response was past experience of a pandemic. In general, in states previously affected by SARS both the public and decision-makers had higher levels of awareness of the need for protective measures and were familiar with social distancing and handwashing procedures, and tests and tracking measures were widely available. Singapore launched a WhatsApp platform with frequent updates, while Taiwan combined national healthcare and immigration databases to generate automated alerts based on travellers’ infection potential, and activated the Central Epidemic Command Centre — created after the SARS epidemic — to coordinate the national effort. All of these initiatives were undertaken even before China had introduced any measures.14
This shows that direct experience of disaster remains the best motivator for systemic preparedness, in seven identifiable ways: prompting thinking and talking; raising awareness and knowledge; helping individuals understand the consequences; developing beliefs; developing preparedness; influencing emotions and feelings; and instigating community interaction on disaster issues.15 Conversely, SARS and the swine flu had negative consequences for European and other states: they served as a blueprint for a virus that peters out before it becomes a global pandemic, or turns out not to be as deadly as initially feared.16 In that sense, they were to some extent dismissed as a false alarm, leading to a reduced threat perception in Europe.
In fact, when taking into account the fact that SARS not only originated in China but was also traced to a wet animal market, Beijing’s response is surprisingly slow. It is worth noting that the WHO, too, was slower in declaring Covid-19 a pandemic than was the case when the swine flu outbreak occurred in 2009.
Defining success in fighting the pandemic
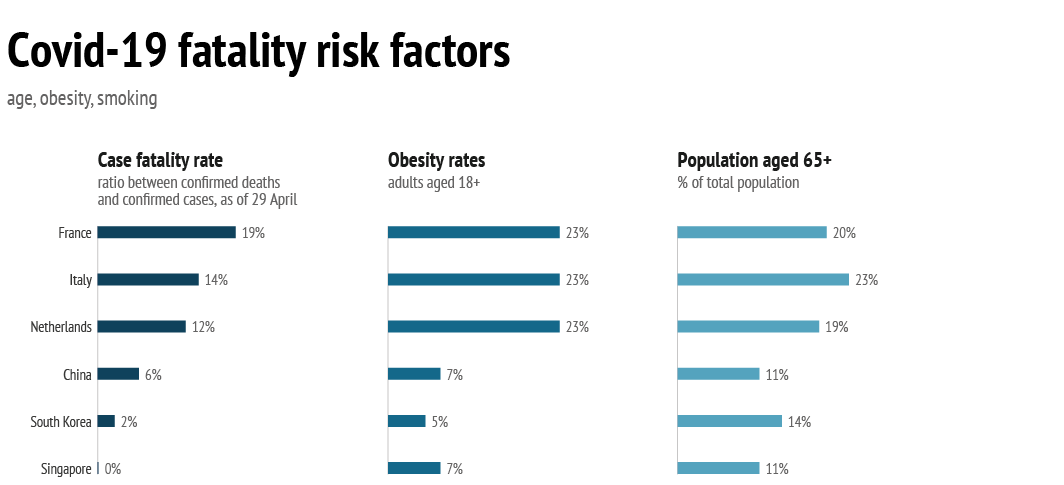
As we have seen, political systems did not play a determining role in the speed of crisis response, but two other factors did: previous first-hand experience of SARS, and high fatality rates. While governments alone are held responsible for high death rates from the virus, elements other than systemic response play a crucial role here, notably the health and age characteristics of a given society – perhaps more than the status of the healthcare system itself. A look at the Global Health Security Index (which measures only systemic dimensions, such as capabilities for prevention, detection, and treatment) shows that, despite being ranked high on the index, certain countries (such as the United States) have in fact displayed high rates of fatality. This is because the index does not include data on population health.18
From a health profile point of view alone, Europe was always going to be at a higher risk than Asian or African countries.
But Covid-19 is particularly lethal in countries with large elderly populations, and that have higher levels of obesity. Initial studies published in early March indicated that the lethality rate among patients aged 70-79 is double that of patients aged 60-69, and more recent statistics from Europe and the United States confirm these findings.19 With nearly 1 in 5 Europeans aged 65 and above, the EU’s population is therefore at greater risk – even though Japan has an even higher population ratio of elderly people, with 28% aged 65 and older. In comparison, in states that had much lower fatality rates – such as South Korea, China and Singapore – the percentage of the population over 65 is correspondingly lower, ranging between 11% and 14%.
But age is not the only determining factor: figures on critical care in the UK show that over 70% of Covid-19 patients were overweight or obese, and health officials in the Netherlands suggest the same.20 This should not have come as a surprise: obesity and excess weight not only impair the immune system – thereby also reducing the effectiveness of antiviral treatments and vaccines – but decrease respiratory function, too, and are often correlated with diabetes (another Covid-19 risk factor). Although surpassed by the US and Canada (which have obesity rates of between 31 and 37%), Europe, too, struggles with this problem, with obesity rates of between 23 and 26%. In comparison, Asian states have much lower obesity rates (between 4 and 7%). From a health profile point of view alone, Europe was always going to be at a higher risk than Asian or African countries.
Data: World Bank, 2019; WHO, 2018; Our World in Data, 2020
Health system resilience, indicating the ability to deal with external shocks, is thus not merely a matter of quality and access; overall population health plays a crucial role too. Unfortunately, Europe was not in good health when the crisis struck: as the Global Trends to 2030 report warned in 2019, many European states were perhaps able to boast good healthcare systems, but not good health practices: 46% of Europeans never exercise.21 The numbers are comparable in the United States, while other countries are doing somewhat better: physical inactivity rates stand at between 29% and 38% in Canada, Iran, South Korea, Japan and Singapore. Only Chinese and Russians appear significantly more active: only 14% of the population in China and 18% of the population in Russia never exercise.22
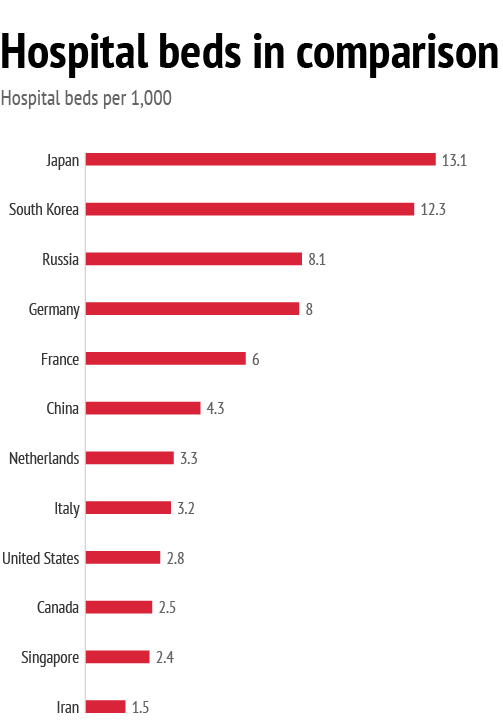
That said, effective government response and the quality of healthcare systems do certainly matter in dealing with health crises. Here, Europe did not perform as well as it might have: between 2000 and 2016, the number of hospital beds per 1,000 people fell in all EU member states, and on average by almost 20%.23 While this reduction can be partly explained by progress in medical technologies cutting down the need for long-term hospitalisation, in many countries the financial and economic crisis of 2008 played a role, too. In some countries, this trend was accompanied by an increase in hospital beds in private for-profit hospitals: in Germany the number of beds in public hospitals fell from 330,000 in 2002 to 270,000 in 2014, while the number of private for-profit beds increased from 170,000 to 200,000. In France, where the number of public hospital beds dropped from 320,000 in 2000 to 260,000 in 2014, during that same period there was only a modest rise from 96,000 to 98,000 private hospital beds.24
To compare: in Russia the number of hospital beds per 1,000 inhabitants was reduced from 11.4 in 2000 to 8.1 in 2017; in Japan from 14.7 to 13.1; and in the US from 3.5 to 2.8. In South Korea and China, the trend was reversed: the number of hospital beds increased from 4.7 to 12.3 and from 1.7 to 4.3, respectively.
Data: OECD, 2017; World Bank, 2020
Policy considerations
Both democracies and authoritarian systems have dealt and continue to deal with the crisis in different ways: no political system has been proved to be demonstrably ‘better’ than another in the swiftness of its response or in reducing the lethal impact of the disease. Instead, previous experience of a similar pandemic, demographic factors and the health status of a population have been of crucial importance in determining how much a state has been affected by the virus. But it must be remembered that, unlike non-democratic systems in China and elsewhere, European democratic systems have to take a more cautious and measured approach in dealing with a pandemic crisis. For instance:
- Certain healthcare measures restrict democratic freedoms, meaning that decision-makers have to persuade the public of the necessity for introducing such measures. While this might take longer than in an authoritarian system, it still has the merit of securing support and compliance.
- A study of Hong Kong’s response to SARS in 2003 showed that the authorities’ purely scientific communication style failed to resonate with a public eager for a more emotional approach highlighting stories of individual courage and heroism, thereby reducing support for the government’s actions. As for the current health crisis, European states, too, initially communicated in a very scientific manner.
- During a pandemic the media play the role of ‘interactive crisis managers’ in democratic systems as they are instrumental in proposing alternative ways out of the crisis, helping interpret the situation, issuing warnings, informing and educating the population, and building support for the government’s strategy.25 But disinformation seeps in as well: the only efficient way to counter this during a crisis is constant, daily and clear communication at the highest possible level.
- Crisis simulation exercises (such as those conducted in 2019 by the EUISS jointly with the Romanian and Finnish Presidencies) can help, but ultimately anticipatory governance is not about focusing on a single event, but rather fostering a general proactive and future-oriented mindset across all governmental sectors. Foresight exercises help in streamlining response mechanisms, but they are not designed to detect early warning signals.26
- While all EU member states have pandemic preparedness plans (although only four of them had updated these in the last five years), this is not the case elsewhere in the world: in the Middle East, for instance, pandemic preparedness is minimal.27 In light of this, health could become a European foreign policy priority.
- Effective warnings need to be precise about the extent and the timing of a crisis (which none of the existing warnings were). But this requires a degree of certainty that is discouraged by our current warning system. Preparing for ‘Grey Rhinos’ (events with a high probability of happening but which we do nothing about because of uncertainty about when they will occur and their full extent) should become a regular feature of governance.28
- Because health is no longer a national affair only, information sharing – both at the global and the European level – will be crucial to meet the next health crisis.
- Health is no longer a purely private matter, but a public international good: states need to take stronger action on preventive measures such as promoting exercise and anti-smoking campaigns.
- Europe was hit at a relatively early stage of the global pandemic. It could turn this situation to its advantage by overcoming the limitations inherent to the crisis mode in which it is currently operating and instead double down on its engagement with those countries and regions that are of strategic importance to Europe. Indeed, in certain ways China’s post-crisis approach may serve as an example.
References
1 Dong Yuzhen, People’s Daily Online, March 4, 2020, http://en.people.cn/n3/2020/0304/c98649-9664589.html.
2 “Democracy, dictatorship, disease: the West takes its turn with Coronavirus”, The Wall Street Journal, March 8, 2020, https://www.wsj.com/articles/democracy-dictatorship-disease-the-west-takes-its-turn-with-coronavirus-11583701472.
3 “The perils of reporting on China’s GDP”, BBC News, January 20, 2017, https://www.bbc.com/news/business-38686570.
4 “Coronavirus: France’s first known case ‘was in December’”, BBC News, May 5, 2020, https://www.bbc.com/news/world-europe-52526554.
5 European Centre for Disease Prevention and Control, “Rapid Risk Assessment: Cluster of pneumonia cases caused by a novel coronavirus, Wuhan, China, 2020”, January 17, 2020, https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-cluster-pneumonia-cases-caused-novel-coronavirus-wuhan.
6 “Coronavirus: Are there two strains and is one more deadly?”, New Scientist, March 5, 2020, https://www.newscientist.com/article/2236544-coronavirus-are-there-two-strains-and-is-one-more-deadly/
7 “How the virus got out”, The New York Times, March 22, 2020, https://www.nytimes.com/interactive/2020/03/22/world/coronavirus-spread.html.
8 “Antibody tests support what’s been obvious: Covid-19 is much more lethal than the flu”, Washington Post, April 28, 2020, https://www.washingtonpost.com/health/antibody-tests-support-whats-been-obvious-covid-19-is-much-more-lethal-than-flu/2020/04/28/2fc215d8-87f7-11ea-ac8a-fe9b8088e101_story.html.
9 “Coronavirus: What are the worst symptoms and how deadly is covid-19?”, New Scientist, March 2, 2020, https://www.newscientist.com/article/2235847-coronavirus-what-are-the-worst-symptoms-and-how-deadly-is-covid-19/#ixzz6L09eKCQE.
10 Data as of 18 May, https://ourworldindata.org/coronavirus
11 No correlation can be found comparing lethality and number of tests conducted per 1,000 inhabitants: in Italy and Spain, these numbers lie between 41 and 47 per 1,000, while the fatality rate is high, too. Conversely, in Canada, the testing rate (31 per 1,000) is relatively high but fatality much lower (7,51%). And while South Korea and the Netherlands have similar test rates (14 and 17 tests per 1,000, respectively), lethality is much higher in the latter country (figures as of 14 May 2020, Our World in Data).
12 Susan D. Moeller, Compassion Fatigue: How the Media Sell Disease, Famine and Death (Routledge: London, 1999), pp.62-4.
13 Center for Infectious Disease Research, “Estimates of SARS death rates revised upward”, May 7, 2003, https://www.cidrap.umn.edu/news-perspective/2003/05/estimates-sars-death-rates-revised-upward.
14 “Singapore Was Ready for Covid-19—Other Countries, Take Note”, Wired, March 12, 2020, https://www.wired.com/story/singapore-was-ready-for-covid-19-other-countries-take-note/
15 Julia Becker et al., “The role of prior experience in informing and motivating earthquake preparedness”, International Journal of Disaster Risk Reduction, March 22, 2017; Roman Hoffmann and Raya Muttarak, “Learn from the Past, Prepare for the Future: Impacts of Education and Experience on Disaster Preparedness in the Philippines and Thailand”, World Development, vol. 96, August 2017, pp. 32-51.
16 France, Germany, Ireland, Italy, Romania, Spain, Sweden and the United Kingdom all reported between 1 and 9 SARS cases, and 0 deaths.
17 David Grimes, “False Alarms and Pseudo-Epidemics: The Limitations of Observational Epidemiology”, Obstetrics & Gynecology, vol. 120, no. 4, October 2012, pp 920-27.
18 “Ranked: Global Pandemic Preparedness by Country”, Visual Capitalist, March 20, 2020, https://www.visualcapitalist.com/global-pandemic-preparedness-ranked/
19 “Estimates of the severity of coronavirus disease 2019: a model-based analysis”, The Lancet, March 30, 2019, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30243-7/fulltext.
20 “Coronavirus: New figures on intensive care deaths revealed”, The Guardian, March 29, 2020, https://www.theguardian.com/society/2020/mar/28/coronavirus-intensive-care-uk-patients-50-per-cent-survival-rate.
21 European Strategy and Policy Analysis System, “Global Trends to 2030: Challenges and Choices for Europe”, April 2019, p. 35, https://www.iss.europa.eu/sites/default/files/EUISSFiles/ESPAS_Report.pdf.
22 World Health Organization, “Noncommunicable diseases country profiles 2018”, https://www.who.int/nmh/publications/ncd-profiles-2018/en/.
23 OECD, “Health at a Glance 2019: OECD Indicators”, OECD Publishing, Paris, 2019, https://doi.org/10.1787/4dd50c09-en.
24 OECD and European Commission, “Health at a Glance: Europe 2016 – State of Health in the EU Cycle”, OECD Publishing, Paris, 2016, http://dx.doi.org/10.1787/9789264265592-en.
25 Chris Hudson, “Singapore at war: SARS and its metaphors”, in John H. Powers & Xiaosui Xiao (eds.), The Social Construction of SARS: Studies of a Health Communication Crisis (Amsterdam/Philadelphia: John Benjamins Publishing Company, 2008), pp.163–80.
26 Daniel Fiott, “Stress tests: An insight into crisis scenarios, simulations and exercises”, EUISS Brief no. 9, September 2019, https://www.iss.europa.eu/content/stress-tests.
27 Wasiq Khan et al., “Influenza pandemic preparedness in the World Health Organization Eastern Mediterranean Region”, Eastern Mediterranean Health Journal, December 2017, http://www.emro.who.int/emhj-volume-25-2019/volume-25-issue-8/influenza-pandemic-preparedness-in-the-world-health-organization-eastern-mediterranean-region.html.
28 Richard A. Clarke and R.P. Eddy, Warnings: Finding Cassandras to Stop Catastrophes (Harper Collins Publishers: New York, 2017), p.224.